PhD proposal
Supervisor: J.E. SARRY
Team J.E. Sarry – CRCT
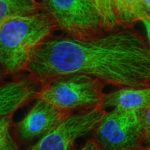
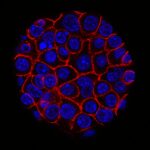
Despite a high rate of complete remission after treatment with genotoxic agents, the prognosis is poor in human acute myeloid leukemia (AML). Front-line chemotherapy is highly effective in ablating leukemic cells, but relapses caused by tumor regrowth initiated by resistant leukemic clones (RLCs) are observed in the majority of patients. The biology of therapeutic resistance currently represents an active area of research. However, the molecular mechanisms underlying drug resistance are still poorly understood in AML, especially in the in vivo context. To address this issue and to characterize chemoresistance and minimal residual disease (MRD), we established a robust patient-derived xenograft (PDX)-based preclinical model that predicts response to chemothepeutics in AML patients. Taking advantage of these in vivo models, we demonstrated that in vivo drug tolerant/resistant AML cells present an enhanced mitochondrial oxidative metabolism. Furthermore, our studies shown that the catabolic flexibility, the inflammatory response, and the metabolic cooperation between stromal and leukemic compartments are key players of mitochondrial activities of chemoresistant AML cells13,14. Therefore our previous results provide not only new targets but also a strong scientific rationale for ongoing clinical trials that assessed emerging combinatory therapies with different mitochondrial inhibitors in AML. Altogether, our work suggests that the mitochondrial function, the metabolic cooperation and symbiosis between the stromal and leukemic compartments inside the bone marrow niche, and inflammatory/stress responses, play a crucial role in drug resistance of AML.
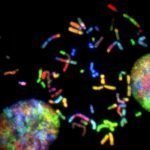
In light of our current results and evidences, our working hypothesis is that the microenvironment-tumor interplay regulates mitochondrial metabolism of AML cells through the activation of key transcriptional factors and regulons, and of stress responses, leading to drug resistance in vivo. To address this hypothesis and to further decipher the heterogeneity of these drug resistance pathways at both single cell and tissue levels, our methodological strategy is based on functional approaches using well-characterized AML cell lines and primary patient samples in vitro and in our xenograft NSG model coupled to bulk and single cell omics and computational approaches. Finally, our preliminary single cell transcriptomic analysis of cells collected from PDX and patients at diagnosis and relapse uncovered a subpopulation endowed with a specific transcriptional profile implicated into (and predictive of) the relapse in AML.
Key Words: AML, drug resistance, metabolism, in silico modeling, computational prediction